Health
‘Rivers Among Best States In Malaria Control’
As the world commemorates another World Malaria Day (WMD) tomorrow, attention is once again drawn to considerations of how far states, regions, and countries have fared in the fight against malaria.
Globally, according to Fact Sheet of the Economic Section of the United States Embassy in Nigeria, malaria affects 3.3 billion people, or half of the world’s population, in 106 countries and territories. The World Health Organisation (WHO) estimates also show that 216 million cases of malaria occurred in 2010, with 81% in the African region.
WHO further estimates that there were 655,000 malaria deaths in 2010, with 91% of it occurring in Africa, and 86% of which were children under 5 years of age. The body also noted that malaria is the 3rd leading cause of death for children under-five years worldwide, after pneumonia and diarrhea disease.
The Economic Section of the United States Embassy in Nigeria also stated that thirty countries in Sub-Saharan Africa account for 90% of global malaria deaths, with Nigeria, Democratic Republic of Congo (DRC), Ethiopia and Uganda accounting for nearly 50% of the global malaria deaths.
Meanwhile, the Fact Sheet noted that malaria is the 2nd leading cause of death from infectious diseases in Africa, after HIV/AIDS and that about 1 out of 5 deaths of children under 5 in Africa are due to malaria.
In Nigeria, according to the Fact Sheet, malaria is a major public health problem and accounts for more cases and deaths than any other country in the world. About 97% of the country’s population is said to be at risk of contacting malaria.
Again, there are an estimated 100 million malaria cases with over 300,000 deaths per year in Nigeria. This is over the estimated 215,000 HIV/AIDS-related deaths per year in the country.
Malaria contributes to an estimated 11% of maternal mortality and accounts for 60% of outpatient visits and 30% of hospitalizations among children under five years of age in Nigeria.
The ailment is said to have the greatest prevalence, with close to 50% in children age 6-59 months in the South West, North Central, and North West regions, while it has the least prevalence (27.6) in children age 6 to 59 months in the South East region.
It is noteworthy that the government at various levels in Nigeria, in collaboration with various implementing partners, have done much in malaria control. In spite of these however, noticeable challenges and gaps still exist.
Such challenges and gaps include poverty being a major factor in malaria prevention and treatment, and that an estimated 65% of Nigeria’s population lives in poverty. Added to this, vector control is highly dependent on pyrethroids, a single class of insecticides, resistance to which has been reported in 27 countries in sub-Saharan Africa, including Nigeria.
Quoting the World Malaria Report of November 2018, the Programme Manager, Rivers State Malaria Elimination Programme, Dr. Mina Jaja said 219 million cases of malaria still occur globally. Out of this, she said, five countries accounted for half of all malaria cases.
“Of these five countries, Nigeria accounted for 25%. So you know what that means. It’s still a course for concern for us in the country”, she said.
In the midst of these realities, Dr. Jaja said, Rivers State has managed to be among the top states known to have performed outstandingly in malaria control since the last WMD in 2018.
“Thankfully, in Rivers State, the prevalence is 7.3% as against the national prevalence of 27%. So, in every sense of modesty, Rivers State ranks among the five best states in malaria control”.
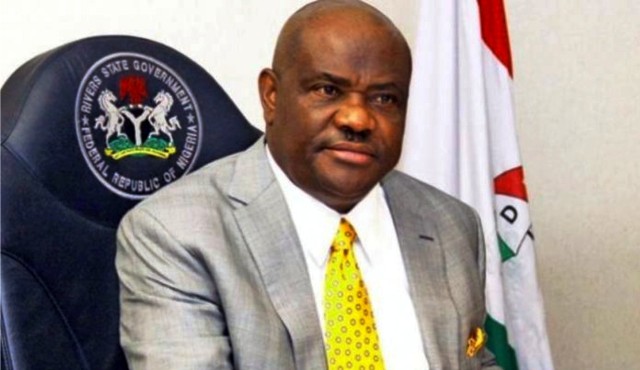
She credits this development to partly the commitment of the state Governor, Nyesom Wike, who, she said, as the Grand Ambassador for Malaria Elimination in the state, “has given us a political platform and stability in the political terrain that has made battling the malaria scourge a little bit easier for us”.
One key contribution of the governor, she hinted, is the renovation and equipment of several health care facilities.
“The renovation and equipping of several secondary health care facilities made it easy for people to access health care. You know, for malaria, you must test before you treat, and you will test when there are facilities where you can go and test. The more facilities you can walk in and test, the better”.
She also credited the efforts of other partners, which include WHO, Shell Petroleum, Development Company (SPDC), and Nigeria Liquefied Natural Gas (NLNG).
From their contributions, she hinted, “there have been a massive scale-up in the various intervention strategies to reduce the burden of malaria (in the state)”, she said.
The peculiarity of the 2019 WAD, Dr. Jaja, explained, is its global theme, “Zero malaria starts with me”, which is further individualised to “Zero malaria starts with me, Join Me” in Nigeria.
“This is individualizing the World Malaria Day, individualizing zero malaria. It emphasises citizen participation. It’s not about moving the buck to the government. It’s about you. So, what are you, as a person, going to do to attain zero malaria?
The WMD was established in May 2007 by the 60th session of the World Health Assembly, which is WHO’s decision-making body. The day was established to provide “education and understanding of malaria” and spread information on “year-long intensified implementation of national malaria-control strategies, including community-based activities for malaria prevention and treatment in endemic areas.”
Before the establishment of WMD, Africa Malaria Day (AMD) was held on April 25. It began in 2001, one year after the historic ”Abuja Declaration” was signed by 44 malaria-endemic countries at the African Summit on Malaria.
WMD allows for corporations, multinational organisations, and grassroots organisations globally to work together to bring awareness to malaria and advocate for policy changes, with each commemoration focusing on a specific theme.
The theme for 2018 was “Ready to beat malaria”, that for 2016 – 2017 was “End Malaria for Good”, while it was “Invest in the future: defeat malaria” in 2013-2014-2015.
Others were: “Sustain Gains, Save Lives: Invest in Malaria” (2012); “Achieving Progress and Impact” (2011); “Counting malaria out” (2009 – 2010); and “Malaria: a disease without borders” (2008).
Events marking the commemoration of the 2019 WMD in Rivers State commenced last Friday with a Jumat service at the Central Mosque, Victoria Street, Port Harcourt. It was followed by LLIN demonstration at Seventh Day Adventist Church, Mile Three, Port Harcourt.
Highlight of tomorrow’s commemoration, which will be the grand finale, will free malaria screening for civil servants and the public at the state Secretariat Complex and massive distribution of LLINs at the venue.
Sogbeba Dokubo
Health
Lagos Trains Health Workers On Handling SGBV Cases
To address the increasing number of rape and defilement cases in Lagos communities, the State Ministry of Health has trained healthcare workers on the prevention and management of sexual assault cases.
The Director, Public Affairs in the ministry, Tunbosun Ogunbanwo, in a statement on Monday said the training equipped health workers with the knowledge and skills to provide professional, compassionate, and timely care to survivors.
Dr Folasade Oludara, Director, Family Health and Nutrition, State Ministry of Health, said the growing number of rape and defilement cases in Lagos communities necessitated the upskilling of healthcare workers who are often the first responders to survivors.
Oludara, represented by Dr Oluwatosin Onasanya, Deputy Director, Child Health, said the government recognised the critical role of health professionals in both clinical management and legal documentation of sexual assault cases.
She explained that the training was designed to ensure healthcare workers are adequately equipped to identify, document, and manage sexual assault cases effectively.
According to her, the training will strengthen Lagos’ coordinated health system response to gender-based violence.
She disclosed that the state government had already provided equipment and specimen collection tools to health facilities, noting that the training complemented this investment by building the competence of personnel handling such sensitive cases.
Oludara explained that doctors and nurses at the primary, secondary, and tertiary levels who serve as first contact points for survivors were carefully selected from all 57 LGAs and LCDAs, particularly from areas with higher incident rates.
The SGBV Programme Manager, Lagos State Ministry of Health, Dr Juradat Aofiyebi, emphasised that the capacity-building initiative was a strategic step toward improving survivor-centred healthcare delivery and prosecution outcomes.
Aofiyebi added that the training underscored the government’s commitment to reducing the prevalence of sexual assault through a robust, multi-sectoral approach.
“The training provides healthcare workers with the knowledge to properly identify survivors, document findings accurately, and provide comprehensive care, all of which contribute to justice delivery and prevention of repeat offences.
She said the ministry would sustain such training to ensure that every survivor who presented at a Lagos health facility received quality, non-judgmental care.
Mrs Adebanke Ogunde, Deputy Director, Directorate of Public Prosecutions (DPP), Lagos State Ministry of Justice, highlighted the importance of medical documentation in sexual assault trials.
She explained that most convictions hinge on the quality of medical reports and forensic evidence provided by healthcare professionals, noting that medical reports served as vital corroborative evidence in court, particularly in cases involving children.
“Your medical reports are crucial; they can determine whether justice is served or denied,” she said.
Ogunde reminded health workers of their legal duty to report suspected sexual assault cases to the police or the Lagos State Domestic and Sexual Violence Agency (DSVA).
Similarly, Dr Oluwajimi Sodipo, Consultant Family Physician, Lagos State University Teaching Hospital (LASUTH), underscored the importance of timely medical attention, psychosocial support, and non-stigmatising care for survivors.
Sodipo explained that immediate presentation within 72 hours of assault improved chances of preventing infections and collecting viable forensic evidence.
He commended Lagos State for sustaining its inter-agency collaboration and continuous professional training on SGBV.
Sodipo, however, called for the strengthening of DNA and forensic capacities, improved insurance coverage, and better remuneration for healthcare workers.
“We must sustain motivation and continuous retraining if we want to retain skilled professionals and enhance justice outcomes,” he added.
Also, Mrs Margret Anyebe, Claims Officer, Lagos State Health Management Agency (LASHMA), said domestic and sexual violence response had been integrated into the ILERA EKO Health Insurance Scheme.
Anyebe explained that survivors of sexual and domestic violence are covered for medical treatment, investigations, and follow-up care under the state’s Equity Fund for vulnerable groups.
“Hospitals are to provide first-line care, document, and refer survivors appropriately, while LASHMA ensures prompt reimbursement and oversight,” she said.
Health
Nch Technical Session Reviews 35 Memos …Sets Stage For Council Deliberations
The technical session of the ongoing National Council on Health (NCH) meeting on Monday reviewed 35 out of the 82 policy memos submitted ahead of full Council deliberations scheduled for later in the week.
Dr Kamil Shoretire, Director of Health Planning, Research and Statistics, disclosed this on Tuesday during the Technical Session of the 66th Regular meeting of the NCH ongoing in Calabar, Cross River.
He said that 10 of the memos considered were recommended for Council’s approval, eight were noted, and 18 stepped down for further work.
According him, two additional memos were deferred and will be re-presented after revisions are made.
At the reconvening of the session, Ms Kachallom Daju, Permanent Secretary, Ministry of Health and Social Welfare, said that there were five memos from the Coordinating Minister of Health, adding that they were all related to the Department of Food and Drugs.
Daju said that the memos were stepped down on Monday and scheduled for re-presentation.
She also provided clarification on the previously contentious healthcare waste-management memo, explaining that the N3.5 million requests tied to the proposal had already been repurposed by the Global Fund.
“I have followed up, and I am informed that the funds have been reprogrammed. Just so we put it to rest, we will not be discussing that memo anymore,” she said.
She also said that the final memo considered on Monday was the proposal for the inclusion of telemedicine services under the National Health Insurance Authority (NHIA).
“The next memo scheduled for presentation is the proposal for the establishment of Medipool as a Group Purchasing Organisation (GPO) for medicines and health commodities in Nigeria.
Meanwhile, Dr Oritseweyimi Ogbe, Secretary of the Ministerial Oversight Committee (MOC), formally notified the Council of the establishment of Medipool, a new public-private GPO created to strengthen the procurement of medicines and health commodities nationwide.
Presenting an information memorandum at the technical session, Ogbe explained that Medipool was the first nationally approved GPO designed to leverage economies of scale, negotiate better prices, and ensure quality-assured medicines.
He said this was beginning with primary healthcare facilities funded through the Basic Health Care Provision Fund (BHCPF).
According to him, Medipool was established after a proposal to the Ministry of Health, followed by appraisals and endorsements by the Project Implementation and Verification Committee (PIVAC) and the Ministry of Finance Incorporated (MOFI).
“It subsequently received Federal Executive Council approval, with MOFI now owning 10 per cent of the company’s shares. The Infrastructure Concession Regulatory Commission has also approved its operations.
“Under the model, Medipool will work with Drug Management Agencies (DMAs) in all states to aggregate national demand and negotiate directly with reputable manufacturers to obtain competitive prices and guaranteed-quality supplies.
“The platform will function as a one-stop shop for DMAs, who will then distribute medicines to health facilities through existing state structures.”
Ogbe added that while Medipool will initially focus on BHCPF-supported primary healthcare centres, it was expected to expand to other levels of care nationwide.
“The organisation will provide regular reports to the ministry of health and participate in national logistics working groups to ensure transparency, oversight, and technical guidance,” he said.
The News Agency of Nigeria (NAN) reports that Day One of the 66th NCH technical session opened with a call reaffirming the Ministry’s commitment to advancing Universal Health Coverage under the theme “My Health, My Right”.
“The delegates also adopted the amended report of the 65th NCH, setting the stage for informed deliberations.
The implementation status of the 19 resolutions from the previous Council was also reviewed, highlighting progress and gaps.
Health
Police Hospital Reports More Malaria Incidence
The authorities of Police Clinic in Port Harcourt have reported high cases of Malaria in its facility.
The revelation was made by Mrs Udoh Mba Robert, a Chief Superintendent of Police and senior medical personnel in the Clinic.
She told The Tide that,”the Hospital admits sixty (60) to seventy (70) patients in a month”.
On how the facility runs, she stated that the hospital is under the National Health Insurance Scheme as most patients are treated almost free.
She maintained that staff of the hospital have been trained professionally to manage health issues that come under the purview of the National Health Insurance Scheme.
Mrs. Robert explained that malaria treatment also falls under NHIA, as patients are expected to pay only 10 per cent for their treatment while the government takes care of the outstanding bills.
NHIA, she further stated covers treatment and care for uniform personnel like the police force, military men, civil servants and all others working for the government.
Urging the public to seek professional medical attention, Mrs. Robert said the facility is open to workers in the federal services, especially police staff.
Favour Umunnakwe, Victory Awaji, Excel Nnodim
-

 Politics4 days ago
Politics4 days agoSenate Urges Tinubu To Sack CAC Boss
-

 News4 days ago
News4 days agoAmend Constitution To Accommodate State Police, Tinubu Tells Senators
-

 News3 days ago
News3 days agoDisu Takes Over As New IGP …Declares Total War On Corruption, Impunity
-
Business4 days ago
Crisis Response: EU-project Delivers New Vet. Clinic To Katsina Govt.
-
Business4 days ago
President Tinubu Approves Extension Ban On Raw Shea Nut Export
-
Business4 days ago
President Tinubu Extends Raw Shea Nuts Export Ban To 2027
-
Business4 days ago
Fidelity Bank To Empower Women With Sustainable Entrepreneurship Skills, HAP2.0
-
Sports4 days ago
NDG: Rivers Coach Appeal To NDDC In Talent Discovery

