Issues
Oil Industry, N’Delta: 20 Years After
These are challenging times for residents of Nigeria’s Niger Delta area. Many leaders in the communities feel a high level of concern about travelling to Port Harcourt through the East-West Road due to the high level of banditry, kidnappings and killings recorded in recent weeks. Indeed, there is a heightened feeling of insecurity in Rivers State, and other Niger Delta communities, as elsewhere in the country. The situation may have gotten worse in the build-up to, and the aftermath of the 2019 General Election.
Let me X-ray emerging issues in the region. It would seem that 20 years after the restoration of civilian rule in Nigeria, we are experiencing worsening human security conditions in this resource-rich region. When a country or state, irrespective of the political system in operation, fails to protect the rights, livelihoods and security of its citizens, then, we have a crisis. What do we do to address the crises that confront us today as a country, particularly in the light of petroleum extraction in the Niger Delta region?
Twenty years ago, as Nigeria was transiting from military dictatorship to civilian rule, the most pressing challenge for the new federal administration was the ecological, human rights and livelihood crises in the oil-bearing Niger Delta region. The members of Niger Delta communities have borne the negative impacts of petroleum extraction. Oil companies operating in the area have historically operated most recklessly. These mostly foreign companies have spilled more crude oil into the natural environment and flared more associated gas here than in any part of the world, resulting in the destruction and degradation of fishing and farming livelihoods, and the increase in diseases and deaths.
Let’s review the issue of community resistance since the 1990s. Of course, the period witnessed the escalation of conflicts between the Nigerian state and petroleum-bearing communities. The oil companies, working with the military regimes at the time, waged a campaign of repression against the community victims of pollution. In our midst today are representatives of the Umuechem community whose plight exemplified the Niger Delta predicament.
In 1990, members of Umuechem community organised a peaceful protest against the pollution of their environment and the destruction of their livelihoods by Shell Petroleum Development Company (SPDC). The community members demanded alternative means of livelihoods and social amenities such as better healthcare. Shell and the Nigerian government responded by sending the Mobile Police to burn down the entire community and kill everyone that they could find in the community. The soldiers spared not even domestic animals in the community. The only survivors of the Umuechem Massacre are people that managed to escape into the bushes. Though, a government enquiry made recommendations for compensation for the survivors, neither the government nor Shell made any restitution. Nobody was charged for the crime, and no one has apologised to the community.
Following the Umuechem Massacre, oil company and government’s repression of peaceful community resistance continued in Ogoniland where many community members were killed, including the leaders of the Movement for the Survival of Ogoni People (MOSOP). All over the Niger Delta region, communities have suffered different forms of human rights abuses and killings because of petroleum extraction. In some cases, such as Rumuekpe in Rivers State, entire towns have been destroyed due to conflicts engineered by oil companies that paid thugs within the community as the companies tried to prevent the people from uniting to demand compensation for pollution and other deprivations.
As a people, it is essential to review the impact of the democratic transition in the last 20 years on the environmental, human rights and development crises in the Niger Delta region. We note that following the General Election of 1999, community members and others expected robust changes in government and companies’ policies and practices to protect the environment, health, livelihoods and other human rights. However, we find that old problems have persisted while new challenges have emerged. For example, in the form of artisanal crude oil refineries, which have provided employment for some youths while exacerbating pollution and insecurity in the region.
We also note that the Federal Government, since 1999, has made some policy and legislative changes and created new institutions such as the Niger Delta Development Commission (NDDC), the Ministry of Niger Delta Affairs (MNDA) and the Presidential Amnesty Programme (PAP). We need to examine the impacts of these institutions and programmes.
Meanwhile, in 2011, the United Nations Environment Programme (UNEP) released a report of its Environmental Assessment of Ogoniland. This report, which confirmed widespread contamination of Ogoniland, made recommendations for immediate environmental and social remediation. The community members hoped that the findings would catalyse fast-tracked action towards ameliorating the problems. However, government response in Ogoniland has been slow and tardy. Elsewhere, there is little or no effort by the Federal Government to address increasing pollution. Recently, the Bayelsa State Government launched an independent commission to examine the impact of oil spills in the state. What is not clear is what role that state governments could play to address an issue under federal jurisdiction.
What is clear, however, is that all tiers of government – federal, state and local – have not always applied petroleum revenues accountably in meeting the development needs of the area. We need to examine what communities and civic organisations should be doing to encourage better accountability in government – beyond participation in voting during elections.
To better clarify the issues, let us dissect the thorny challenge of petroleum legislations at the National Assembly. Today, there is still no legislation that bans gas flaring and protects residents even when communities do not have access to electricity which could be generated from flared gas. The reality of continuing gas flaring underscores the failure of democratic institutions to adequately address the environmental challenges faced by communities in the Niger Delta.
The Senate, in particular, aborted attempts to pass legislation against gas flaring. Also, efforts to pass the Petroleum Industries Bill (PIB) have failed since 2008 due, in part, to contentions over rights of communities in sites of extraction. Later, the Petroleum Industries Governance Bill (PIGB), which contains many problematic provisions, was passed by the National Assembly but rejected by President Muhammadu Buhari. Our organisation called on the President to reject the PIGB, which contains many provisions that would undermine environmental regulations and increase corruption in the petroleum sector. Other bills (that were part of the original PIB) that are still pending before the National Assembly include the Petroleum Host and Impacted Communities Bill (PHICDB), Petroleum Industry Administration Bill (PIAB) and the Petroleum Industry Fiscal Bill (PIFB).
Now, let us examine those proposed legislations, particularly from the point of view of the communities, and make recommendations. I had earlier made reference to Umuechem, which like numerous other communities in the Niger Delta, demand justice. With the historical and continuing failings of the executive and legislative arms of government, oil-bearing communities continue to seek justice through the judiciary with limited results. Communities do not always have the resources for prolonged litigation in Nigeria while a few, often with the support of international NGOs, have attempted international litigation in the home countries of foreign oil companies, with varied results.
Just on May 1, 2019, a court in The Netherlands ruled that it has jurisdiction to determine the complicity of Royal Dutch Shell in the Nigerian government’s murder of the Ogoni Nine leaders of MOSOP who were campaigning against widespread environmental pollution, and for community self-determination. That ruling adds to the judgment of a UK court against SPDC in 2016, in the suit instituted by Bodo community, and opens up possibilities for other victims of pollution and human rights violations.
Now, let us examine workable options for litigation to achieve justice for community victims in areas where petroleum extraction has negatively impacted the people. The Nigeria Resource Justice Conference, 2019 provided a platform for interaction among community members and leaders, citizens groups, scholars, government agencies and elected representatives of the people. Unlike other conferences of this nature, the conference panels bring together experts, activists, agencies and the victims of environmental pollution from the communities.
The conference provided opportunities for participants to dissect the issues of concern to their communities with a view to finding lasting solutions to them, going forward. I think it is important that Niger Delta communities continue to partner NGOs and civil society groups to achieve peace and development in the region by ensuring justice for all victims of the consequences of petroleum extraction activities in the region.
Of particular note is the muscle that a renowned NGO – Development and Peace – has brought to ensure access to justice for Umuechem and other communities. We believe that with further collaboration, other communities’ cries for help will also be remedied.
By: Dr. Isaac Osuoka
Issues
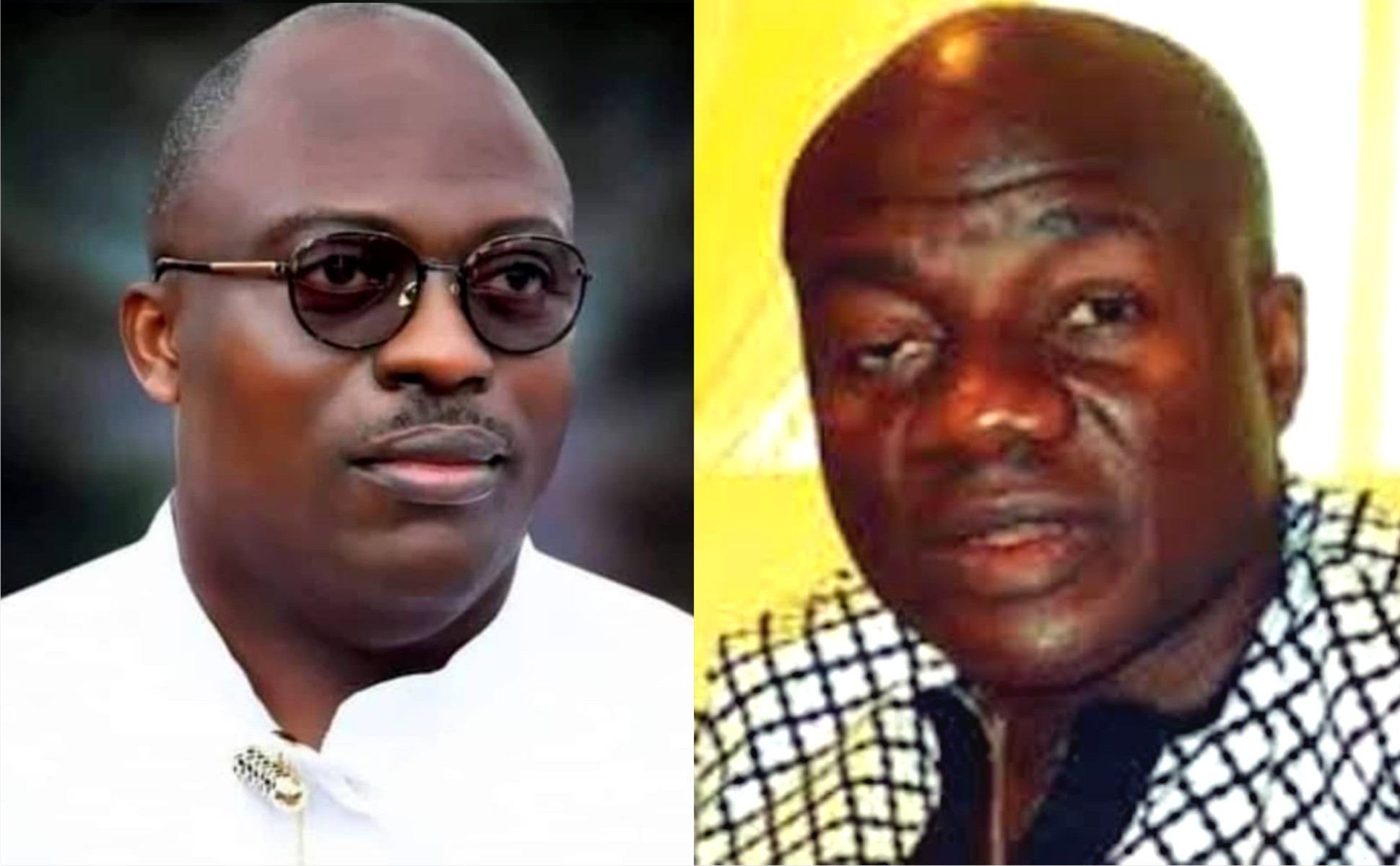
Wike: Destroying Rivers State And PDP
This is an open letter to the Minister of the Federal Capital Territory, Chief Nyesom Wike.
Your Excellency,
Sir, ordinarily, I would not be writing an open letter to you, but like a wise man once said, “Silence would be Treason.” So I prefer to stay alive than face the consequences of silence in the face of crime. With each passing day, and as the socio-political tides continue to turn, it has become more pertinent that more people speak up in a concerted MANNER to prevent the death of our party, the Peoples Democratic Party (PDP), as we appear to be, in the words of W. B. Yeats, “turning and turning in the widening gyre” heading for an end where the falcon will no longer hear the falconer
It is unfortunate that since losing control of the Federal Government, with the loss of President Goodluck Jonathan at the poll in 2015, our party, the Peoples Democratic Party (PDP), has continued on a downward spiral. It is much more painful, that where it is expected that leaders within the party should rise to the challenge and put an end to this decline of our great party, some have instead taken up roles as its undertaker.
It will be hypocritical to claim aloofness to what I believe is your grouse with the PDP and I am not a hypocrite. It will be uncharitable on my part to discountenance the role you have played in strengthening the PDP from 2015 up until the last Presidential primaries of the party. It is my belief that your grouse against certain members of the party who you perceived worked against the party and abandoned it in 2015 and then came around much later to take control of the party, is justified. Also know that your decision to remain in the Party and stifle its progress on the other hand, as a sort of payback, stands condemned. For a man of your pedigree and stature, it is a dishonorable act, highly dishonorable and stands as testimony against all you claim to stand for.
At least, it can be argued that those who you hold this grudge against, abandoned the party completely and did not sit back while actively working to destroy it from within. But what then can be the argument on your own part, seeing that those you are currently working with against your party are the same people who set in motion, and executed surgically, the plans that not only ended our Party’s leadership at the centre, but ended up dislodging the first Niger Deltan to occupy Aso Rock as Commander in Chief of the Armed Forces. Is this not akin to “cutting off one’s nose to spite one’s face?” That will be worse than folly. Let us not throw away the baby with the bath water because we do not like the soap used in bathing the baby. It will be a grave mistake.
Honourable Minister, sir, it is rather unfortunate that of all people, you have also decided to play the role of an undertaker not only for our party, but for our dear Rivers State.
I will like to take you down memory lane a little. Let me remind you of your emergence as Guber candidate of the PDP in Rivers State, against all fairness and justice in 2014. You will remember that despite the reality being that you as an Ikwerre man was poised to replace a fellow Ikwerre man in Governor Chibuike Rotimi Amaechi in our multiethnic state, Rivers people overwhelmingly stood by you and pushed for your emergence as Executive Governor of Rivers State in 2015. I dare say that your popularity in the entire Niger Delta region was at an all-time high at this point.
I want you to understand why you were loved across board leading to your eventual emergence as Governor of Rivers State in 2015; it was because when it looked like all were against the second term ambitions of the first Niger Delta man to emerge as President of Nigeria, you became not just a pillar but a beacon of resistance by standing for Goodluck Jonathan. Rivers people, as grateful and rewarding as they can be, paid you back by ensuring your electoral victory against the incumbent All Progressives Congress (APC) led by your predecessor. On your emergence, where there were second term Governors in the region, you, a first term Governor, was seen by the people as not just the leader of the PDP, but the leader of the entire Niger Delta region. You earned it, and no one could dispute it.
In 2019, when your re-election bid was being challenged ferociously, Rivers people once again stood solidly behind you. Many were killed in the process of defending your votes. Do you remember Dr. Ferry Gberegbe that was shot and killed while trying to protect your votes in Khana Local Government Area? There are many more unnamed and unrecognised sons and daughters of Rivers State who sacrificed their lives so that you could emerge as a second term Governor of Rivers State.
In 2022/23, Honourable Minister, you oversaw a party primary across board that saw some candidates imprisoned and internal party democracy jettisoned for your wishes, leading to the emergence of flag bearers of our party all singlehandedly picked by you. You have on more than one occasion publicly stated that you paid for all their forms. Even those shortchanged in this process licked their wounds and continued to play their roles as party members to ensure the success of the party at all levels. In what will go down as one of the most keenly contested elections in recent Rivers history, with formidable candidates like Senator Magnus Abe of the Social Democratic Party (SDP), Mr Tonye Cole of the All Progressives Congress (APC), and the vibrant youth driven Labour Party (LP), PDP emerged victorious across board except for Phalga Constituency 1 that was lost to the Labour Party. (Not that you did not loose in some other LGA’s but let’s stick to the official figures declared by INEC).
It begs the question, why then do you want to burn down Rivers State, when everyone who now holds political office emerged through a process designed and endorsed by you? Is it that you do not care about Rivers people and you are all about yourself? If so, I am forced to believe that those around you are not telling you the truth. The truth being that in a state where your words were law; where houses and businesses could be demolished or closed down without any recourse to legalities, where Executive Orders could be deployed to stifle the opposition, that your popularity is now at an all-time low. Probably because they are afraid of you, or of losing the benefits they gain from you, they fail to tell you that what you might perceive as a battle against your successor, has slowly but gradually degenerating into a battle against Rivers State and Rivers people. You know, there is a popular saying that, a man can cook for the community and the community will finish the food, but when a community decides to cook for one man, the reverse is the case.
LEAVE FUBARA ALONE
You have gone on and on about being betrayed by Governor Siminalayi Fubara. You point fingers forgetting that some of those same fingers quick to spot betrayals point straight back at you. It is not Governor Fubara that has betrayed the PDP by working against it in the just concluded General Election, and working with the opposition at the State and Federal level to destabilise the party. It is you, Honourable Minister. It is not Governor Fubara that betrayed Rivers people by instigating a political crisis with propensity to escalate ethnic tensions in Rivers State. It is you Honourable Minister. It is not Governor Fubara that has declared himself God over all in Rivers State and has no qualms with burning the state to the ground to prove a point. It is you Honourable Minister. It is you Honourable Minister who told the world that the APC was a cancer and you can never support a cancerous party. It is you Honourable Minister who ended up facilitating the emergence of the same “cancerous” APC that has accelerated the economic decline of this country and further impoverished our people with no remorse. All so you can be a Minister of the Federal Capital Territory? The lack of self awareness is gobsmacking.
Some days back I came across a video where you talked about death and how you do not cry when you hear about the death of some people because you have no idea what might have caused it considering many a politician swear “over dead bodies” and still go back on their words. Those words made me think, and I could see the reason behind them. You see, in chosing to be God in the affairs of Rivers people, you have closed your eyes and ears to reason; you see nothing and hear nothing that can cause you to rethink on the path you have chosen. In your quest to “show Fubara” you have unwittingly united a vast majority of Rivers people behind him, so much that even those who despised him because of you, now like or love him, because of you too. In your scheming, I will advise you not to forget that “the voice of the people is the voice of God”.
Note that the war which you have or are waging against Governor Fubara, has gone beyond being merely political as you might see in your minds eye. It is now one that, fortunately for some and unfortunately for others, has evolved into a war against Rivers people. It is good to point out that no one has taken a stand against Rivers people and won. No one has gone against God and won. In your defiant characteristic manner, it will be unfortunate if you believe your own hubris and that of those around you on the possibility of you being the first to successfully go against Rivers people. It will be a needless gamble; one where if you win you create more enemies for yourself than you can withstand on your political journey, and if you lose, your legacy becomes an inglorious and irredeemable one in Rivers State, the Niger Delta, and Nigeria at large. For your sake as regards posterity, it is my greatest wish that you have a moment of sobriety and a deep reflection and introspection on this path you have chosen.
Honourable Minister, sir, what is left of your legacy is on the brink of being completely desecrated and relegated to the dustbin of our political history, and it will be a sad end to what I will say has been a wonderful political career that many can only dream of. The ball is in your court, and may God Almighty have mercy on us all and forgive us for our shortcomings.
Gabriel Baritulem Pidomson
Dr Pidomson is former Chief of Staff, Government House, Port Harcourt and former member, Rivers State House of Assembly.
Issues
Investing In Nyesom Wike: A Story Of Dedication, Sacrifice And Ultimate Loss

In 2015, I made a conscious decision to invest my financial resources, my time, and energy into supporting Nyesom Wike’s gubernatorial campaign. I poured my heart and soul into ensuring Nyesom Wike emerged victorious even at the risk of my personal safety.
Again in 2019, I doubled down on my commitment. I invested a significant amount of money to procure campaign outfits for all twenty-three Local Governments Areas of Rivers State. I spared no expense in supplementing Wike’s election efforts in my own local government, and once again putting myself at great risk to safeguard the fairness and transparency of the electoral process.
However, despite my unwavering loyalty and sacrifices, I found myself abandoned and forgotten by Wike. Throughout his eight-year tenure, he failed to acknowledge my contributions or fulfill his promises and agreements. Even as a former Deputy Governor, Wike denied me my severance benefit.
My investment in Wike’s governorship was not just financial – it was a commitment of passion, dedication, and belief in a better future for Rivers State. Yet, his leadership style of dishonesty, greed, drunkenness and rash abuse of senior citizens brought me nothing but disappointment, misery and losses.
By the grace of God, today I speak not as a victim, but as a hero. I have accepted my losses, and I have moved on. And as I reflect on my experience, I cannot help but urge Wike to do the same and allow peace and development to reign in Rivers State.
Nyesom Wike, when you speak of investing in Governor Sim Fubara’s election, remember those like me who also invested in you. Remember the sacrifices I made, the risks I took, and the promises and agreements you left unfulfilled.
It is time for you, Wike, to let go of the past and allow Governor Sim Fubara the breathing space he needs to lead Rivers State forward. Allow him to focus on the challenges of good governance and the aspirations of the people. Spare him these unwarranted and ill-conceived political manoeuvrings founded on personal agenda and not for general good of Rivers State and her people.
I may have lost my investment on Wike, but I have not lost hope in the future of Rivers State. And together, we will continue to strive for a brighter tomorrow.
Long Live the Governor to Rivers State, Sir Siminialayi Fubara!
Long Live the Good People of Rivers State!!
Long Live the Federal Republic of Nigeria!!!
Engr Ikuru is former Deputy Governor of Rivers State.
Tele Ikuru
Issues
Is Okocha A Happy Man Being Perpetual Hireling?