Issues
How Accessible Is National Health Insurance Scheme?

Since it became operational in 2005, the National Health Insurance Scheme (NHIS) has been contending with many challenges in the course of defining its objective of making healthcare accessible and affordable to Nigerians.
The scheme has Formal Sector Social Health Insurance Programme which covers the federal, state and local governments as well as the organised private sector.
It also has Informal Sector Social Health Insurance Programme which covers the Community-Based Social Health Insurance Programme and the Voluntary Contributors Social Health Insurance Programme.
The third category is the Vulnerable Group Social Health Insurance Programme which covers the physically challenged persons, prison inmates, children under five, pregnant women and immigrants, among others.
Analysts, however, note that lack of political will, inefficiency of the regulatory agency, the Health Maintenance Organisations (HMOs) and optional enrollment policy, among others, remain contending issues that the scheme has been grappling with in recent times.
According to them, one of the issues is the role of HMOs that are privately owned but play an important role in the operation of the scheme.
They note also that there is a service-gap with the public hospitals that have the distribution of enrollees, playing a dominant role in its healthcare delivery.
They cite instances when enrollees have complained of poor service delivery with long waiting time, use of substandard drugs and poor attitude of healthcare providers.
Concerned citizens have also expressed grave concern that the primary purpose of the scheme, which is to make healthcare financially available and affordable to all Nigerians, is seemed to have been compromised.
Besides this, they note that out-of-pocket payment for healthcare services has, indeed, been a challenge in Nigeria as such affects the ability of households and individuals to meet basic needs.
However, the management of NHIS says it has been making efforts at ensuring commitment and political will to achieve Universal Health Coverage as recommended by the World Health Organisation.
Malam Attahiru Ibrahim, former Executive Secretary of NHIS, said that 98 per cent of the Formal Sector Social Health Insurance Programme has been covered.
“One of our mandates in the scheme is to cover the formal sector and presently we have covered 98 per cent of the work force at the federal level.
“The formal sector consists of the public sector, organised private sector, armed forces, police and other uniformed services,’’ Ibrahim said.
Prof. Usman Yusuf, Executive Secretary, NHIS, nonetheless, acknowledged that the major challenge in the accessibility of health insurance to many Nigerians was the inability to extend the benefit package to the informal sector.
Yusuf also expressed his determination to reposition the scheme to deliver healthcare for all Nigerians, especially to the poor and vulnerable in the society.
He said that the scheme would design and implement strategies that would make NHIS a good steward of the nation’s commonwealth.
He stated that the Community-Based Social Health Insurance Programme with a well-developed design and implementation manual in place was a strategy to reach out to the informal sector.
“So far, more than 48 Community-Based Social Health Insurance Programmes are operational in Nigeria.
“The scheme has inaugurated the programmes in Emoriko and Egbe both in Kogi State, Nkana West Ward 11 of Akwa Ibom, Lamodi-Offa in Kwara and Igarra in Edo, among others.
“The Tertiary Institutions Social Health Insurance Programme, Voluntary Contributors Social Health Insurance Programme and private health plans are part of the programmes to boost health coverage by the scheme,’’ he said.
According to him, the Federal Capital Territory, Kwara, Lagos, Delta, Cross River, Kano, Kebbi, Plateau, Gombe, Osun, Imo and Rivers States have adopted the scheme to boost access to healthcare services.
Similarly, Dr Emmanuel Uba, General Manager, Formal Sector Department, said that the Vital Contributor’s Social Health Insurance Programme was designed to cover the healthcare needs of senior citizens, retirees, aged and Nigerians who are not on the platform of NHIS.
“The programme allows individuals to pay N15, 000 annually for their own contributions, renewable annually and provides access to quality healthcare services for the enrollees.
“NHIS is a contributory scheme, which means, is either you contribute or someone else contributes on your behalf which keeps you covered.
“When people retire from service, they are out of government payroll and they do not contribute to the contributory fund. This programme, therefore, enables them to have access to healthcare after retirement.
“Also for the vulnerable groups to have access to healthcare insurance there is need for equity funds that would cater for the vulnerable group such as the physically challenged persons, prison inmates, children less than five years of age, pregnant women and immigrants, among others.
“There is also need to explore Innovative Financing where various companies such as telecommunications, beverages and alcohol companies can be taxed and some percentage could go into the pool for the vulnerable groups.
“For this to work we will need a legislation by the National Assembly, the president’s assent to it as well as the support from stakeholders and political will from the state government,’’ Uba said.
To ensure unhindered access to healthcare services, Mr Roberts Ukeje, FCT Chapter Manager, Managed Healthcare Services, a HMO, sought the cooperation of enrollees to give feedback on service delivery in healthcare facilities and to insist on their rights to quality healthcare.
He said that regular feedback by enrollees would enhance improvement on services as well as quality standard in hospitals across the country.
He noted that there ought to be feedback from enrollees on their experiences at service delivery points and health facilities to assist the scheme in sustaining and improving quality healthcare.
Ukeje also said that every enrollee registered in the scheme had a right to access medical treatment as outlined in the NHIS benefit package, “such as the right to select a healthcare facility of their choice as long as the facility is accredited by the scheme.
“The right to change a primary healthcare facility after six months of access if not satisfied with the services provided and the right to choose an alternative facility for dependents if they are living in a different location, among others’’
Tola writes for the News Agency of Nigeria.
Mohammad Tola
Issues
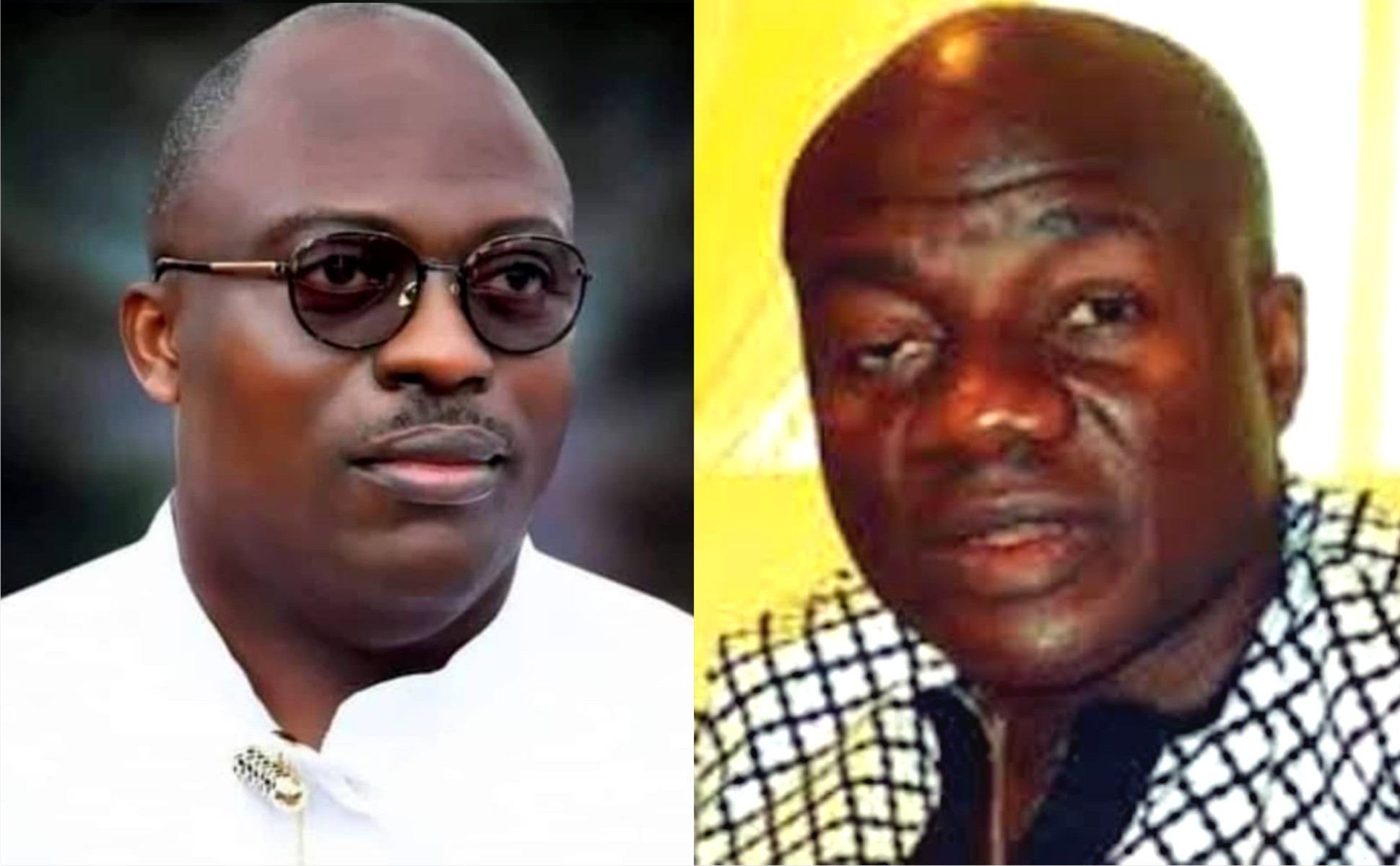
Wike: Destroying Rivers State And PDP
This is an open letter to the Minister of the Federal Capital Territory, Chief Nyesom Wike.
Your Excellency,
Sir, ordinarily, I would not be writing an open letter to you, but like a wise man once said, “Silence would be Treason.” So I prefer to stay alive than face the consequences of silence in the face of crime. With each passing day, and as the socio-political tides continue to turn, it has become more pertinent that more people speak up in a concerted MANNER to prevent the death of our party, the Peoples Democratic Party (PDP), as we appear to be, in the words of W. B. Yeats, “turning and turning in the widening gyre” heading for an end where the falcon will no longer hear the falconer
It is unfortunate that since losing control of the Federal Government, with the loss of President Goodluck Jonathan at the poll in 2015, our party, the Peoples Democratic Party (PDP), has continued on a downward spiral. It is much more painful, that where it is expected that leaders within the party should rise to the challenge and put an end to this decline of our great party, some have instead taken up roles as its undertaker.
It will be hypocritical to claim aloofness to what I believe is your grouse with the PDP and I am not a hypocrite. It will be uncharitable on my part to discountenance the role you have played in strengthening the PDP from 2015 up until the last Presidential primaries of the party. It is my belief that your grouse against certain members of the party who you perceived worked against the party and abandoned it in 2015 and then came around much later to take control of the party, is justified. Also know that your decision to remain in the Party and stifle its progress on the other hand, as a sort of payback, stands condemned. For a man of your pedigree and stature, it is a dishonorable act, highly dishonorable and stands as testimony against all you claim to stand for.
At least, it can be argued that those who you hold this grudge against, abandoned the party completely and did not sit back while actively working to destroy it from within. But what then can be the argument on your own part, seeing that those you are currently working with against your party are the same people who set in motion, and executed surgically, the plans that not only ended our Party’s leadership at the centre, but ended up dislodging the first Niger Deltan to occupy Aso Rock as Commander in Chief of the Armed Forces. Is this not akin to “cutting off one’s nose to spite one’s face?” That will be worse than folly. Let us not throw away the baby with the bath water because we do not like the soap used in bathing the baby. It will be a grave mistake.
Honourable Minister, sir, it is rather unfortunate that of all people, you have also decided to play the role of an undertaker not only for our party, but for our dear Rivers State.
I will like to take you down memory lane a little. Let me remind you of your emergence as Guber candidate of the PDP in Rivers State, against all fairness and justice in 2014. You will remember that despite the reality being that you as an Ikwerre man was poised to replace a fellow Ikwerre man in Governor Chibuike Rotimi Amaechi in our multiethnic state, Rivers people overwhelmingly stood by you and pushed for your emergence as Executive Governor of Rivers State in 2015. I dare say that your popularity in the entire Niger Delta region was at an all-time high at this point.
I want you to understand why you were loved across board leading to your eventual emergence as Governor of Rivers State in 2015; it was because when it looked like all were against the second term ambitions of the first Niger Delta man to emerge as President of Nigeria, you became not just a pillar but a beacon of resistance by standing for Goodluck Jonathan. Rivers people, as grateful and rewarding as they can be, paid you back by ensuring your electoral victory against the incumbent All Progressives Congress (APC) led by your predecessor. On your emergence, where there were second term Governors in the region, you, a first term Governor, was seen by the people as not just the leader of the PDP, but the leader of the entire Niger Delta region. You earned it, and no one could dispute it.
In 2019, when your re-election bid was being challenged ferociously, Rivers people once again stood solidly behind you. Many were killed in the process of defending your votes. Do you remember Dr. Ferry Gberegbe that was shot and killed while trying to protect your votes in Khana Local Government Area? There are many more unnamed and unrecognised sons and daughters of Rivers State who sacrificed their lives so that you could emerge as a second term Governor of Rivers State.
In 2022/23, Honourable Minister, you oversaw a party primary across board that saw some candidates imprisoned and internal party democracy jettisoned for your wishes, leading to the emergence of flag bearers of our party all singlehandedly picked by you. You have on more than one occasion publicly stated that you paid for all their forms. Even those shortchanged in this process licked their wounds and continued to play their roles as party members to ensure the success of the party at all levels. In what will go down as one of the most keenly contested elections in recent Rivers history, with formidable candidates like Senator Magnus Abe of the Social Democratic Party (SDP), Mr Tonye Cole of the All Progressives Congress (APC), and the vibrant youth driven Labour Party (LP), PDP emerged victorious across board except for Phalga Constituency 1 that was lost to the Labour Party. (Not that you did not loose in some other LGA’s but let’s stick to the official figures declared by INEC).
It begs the question, why then do you want to burn down Rivers State, when everyone who now holds political office emerged through a process designed and endorsed by you? Is it that you do not care about Rivers people and you are all about yourself? If so, I am forced to believe that those around you are not telling you the truth. The truth being that in a state where your words were law; where houses and businesses could be demolished or closed down without any recourse to legalities, where Executive Orders could be deployed to stifle the opposition, that your popularity is now at an all-time low. Probably because they are afraid of you, or of losing the benefits they gain from you, they fail to tell you that what you might perceive as a battle against your successor, has slowly but gradually degenerating into a battle against Rivers State and Rivers people. You know, there is a popular saying that, a man can cook for the community and the community will finish the food, but when a community decides to cook for one man, the reverse is the case.
LEAVE FUBARA ALONE
You have gone on and on about being betrayed by Governor Siminalayi Fubara. You point fingers forgetting that some of those same fingers quick to spot betrayals point straight back at you. It is not Governor Fubara that has betrayed the PDP by working against it in the just concluded General Election, and working with the opposition at the State and Federal level to destabilise the party. It is you, Honourable Minister. It is not Governor Fubara that betrayed Rivers people by instigating a political crisis with propensity to escalate ethnic tensions in Rivers State. It is you Honourable Minister. It is not Governor Fubara that has declared himself God over all in Rivers State and has no qualms with burning the state to the ground to prove a point. It is you Honourable Minister. It is you Honourable Minister who told the world that the APC was a cancer and you can never support a cancerous party. It is you Honourable Minister who ended up facilitating the emergence of the same “cancerous” APC that has accelerated the economic decline of this country and further impoverished our people with no remorse. All so you can be a Minister of the Federal Capital Territory? The lack of self awareness is gobsmacking.
Some days back I came across a video where you talked about death and how you do not cry when you hear about the death of some people because you have no idea what might have caused it considering many a politician swear “over dead bodies” and still go back on their words. Those words made me think, and I could see the reason behind them. You see, in chosing to be God in the affairs of Rivers people, you have closed your eyes and ears to reason; you see nothing and hear nothing that can cause you to rethink on the path you have chosen. In your quest to “show Fubara” you have unwittingly united a vast majority of Rivers people behind him, so much that even those who despised him because of you, now like or love him, because of you too. In your scheming, I will advise you not to forget that “the voice of the people is the voice of God”.
Note that the war which you have or are waging against Governor Fubara, has gone beyond being merely political as you might see in your minds eye. It is now one that, fortunately for some and unfortunately for others, has evolved into a war against Rivers people. It is good to point out that no one has taken a stand against Rivers people and won. No one has gone against God and won. In your defiant characteristic manner, it will be unfortunate if you believe your own hubris and that of those around you on the possibility of you being the first to successfully go against Rivers people. It will be a needless gamble; one where if you win you create more enemies for yourself than you can withstand on your political journey, and if you lose, your legacy becomes an inglorious and irredeemable one in Rivers State, the Niger Delta, and Nigeria at large. For your sake as regards posterity, it is my greatest wish that you have a moment of sobriety and a deep reflection and introspection on this path you have chosen.
Honourable Minister, sir, what is left of your legacy is on the brink of being completely desecrated and relegated to the dustbin of our political history, and it will be a sad end to what I will say has been a wonderful political career that many can only dream of. The ball is in your court, and may God Almighty have mercy on us all and forgive us for our shortcomings.
Gabriel Baritulem Pidomson
Dr Pidomson is former Chief of Staff, Government House, Port Harcourt and former member, Rivers State House of Assembly.
Issues
Investing In Nyesom Wike: A Story Of Dedication, Sacrifice And Ultimate Loss

In 2015, I made a conscious decision to invest my financial resources, my time, and energy into supporting Nyesom Wike’s gubernatorial campaign. I poured my heart and soul into ensuring Nyesom Wike emerged victorious even at the risk of my personal safety.
Again in 2019, I doubled down on my commitment. I invested a significant amount of money to procure campaign outfits for all twenty-three Local Governments Areas of Rivers State. I spared no expense in supplementing Wike’s election efforts in my own local government, and once again putting myself at great risk to safeguard the fairness and transparency of the electoral process.
However, despite my unwavering loyalty and sacrifices, I found myself abandoned and forgotten by Wike. Throughout his eight-year tenure, he failed to acknowledge my contributions or fulfill his promises and agreements. Even as a former Deputy Governor, Wike denied me my severance benefit.
My investment in Wike’s governorship was not just financial – it was a commitment of passion, dedication, and belief in a better future for Rivers State. Yet, his leadership style of dishonesty, greed, drunkenness and rash abuse of senior citizens brought me nothing but disappointment, misery and losses.
By the grace of God, today I speak not as a victim, but as a hero. I have accepted my losses, and I have moved on. And as I reflect on my experience, I cannot help but urge Wike to do the same and allow peace and development to reign in Rivers State.
Nyesom Wike, when you speak of investing in Governor Sim Fubara’s election, remember those like me who also invested in you. Remember the sacrifices I made, the risks I took, and the promises and agreements you left unfulfilled.
It is time for you, Wike, to let go of the past and allow Governor Sim Fubara the breathing space he needs to lead Rivers State forward. Allow him to focus on the challenges of good governance and the aspirations of the people. Spare him these unwarranted and ill-conceived political manoeuvrings founded on personal agenda and not for general good of Rivers State and her people.
I may have lost my investment on Wike, but I have not lost hope in the future of Rivers State. And together, we will continue to strive for a brighter tomorrow.
Long Live the Governor to Rivers State, Sir Siminialayi Fubara!
Long Live the Good People of Rivers State!!
Long Live the Federal Republic of Nigeria!!!
Engr Ikuru is former Deputy Governor of Rivers State.
Tele Ikuru
Issues
Is Okocha A Happy Man Being Perpetual Hireling?
The man Tony Okocha, the devastated tattered ragtag remnant Rivers APC factional, but Caretaker, Chairman, is known for being notoriously a hireling willing to play in the mud just for the pay or settlement. To Rt Hon Chibuike Rotimi Amaechi, he did against Chief Nyesom Wike. To Senator Magnus Abe, he did against Rotimi Amaechi. To Chief Nyesom Wike, he did against Magnus Abe. Having maintained such unbefitting character trait, it is not surprising to see him at his demeaned best showing off his tainted skill of grandstanding and loquaciously struggling fruitlessly almost every day to castigate the popular Rivers people’s Governor with very glaring false, bogus and unsubstantiated claims such as:
1. That Governor Fubara is wasting state fund in the name of thanksgiving across 23 Local Government Areas.
2. That Governor Fubara has withheld Local Government funds.
3. That Governor Fubara runs the government without input from the State Executive Council.
4. That nothing is happening in the State with respect to governance.
To the above false claims of Tony Okocha, every reasonable, right thinking and well-meaning Rivers person would effortlessly puncture all as rascality and mendacity taken too far.
Apart from the fact that Governor Siminalayi Fubara had said he is not sponsoring the massive SIMplified Movement Thanksgiving events across the Local Government Areas of the State being organised by elated Rivers people who feel liberated from an era of overbearing and suppressive form of leadership in the State, Tony Okocha should be asked to prove his false claim with indisputable facts and figures. Until then, let Tony Okocha respect himself and learn to keep quiet as an elderly person who is saddled with such a responsible position as Rivers State Representative in the Niger Delta Development Commission (NDDC) Board. A position that places a huge responsibility on him to ensure that the core objectives of the commission are actualised in the State, by not only ensuring that Rivers State gets its fair share of its dues in terms of projects, programmes and activities, but by synergising with the state government on development matters concerning the state vis-a-vis the responsibilities of NDDC to the State. In summary, the SIMplified Movement is all about a happy and joyful people of Rivers State who have decided to stand and stick together to defend and uphold their common heritage and patrimony. It is a voluntary venture, not sponsored by the government.
To his claim that the Governor has withheld Local Government funds, Mr Tony Okocha should also be asked to prove that with facts and figures and explain why the Governor would do such. More so, what is Tony Okocha’s business, assuming, but not conceding, that a PDP Governor withholds money against PDP-led 23 Local Government authorities? Did Local Government workers across the state complain to Okocha, the meddlesome hireling, an acclaimed APC Caretaker Committee Chairman in Rivers State?
On his ignorant and false claim that the Governor runs the government without input from the state exco, Okocha, the busybody wannabe should explain how he was employed or engaged as the spokesperson of members of the Rivers State Executive Council. He should also tell us his source of information to that effect, if it is not just a proof that he is making himself known as a perpetually irredeemable hireling notoriously good for playing the spoiler’s role.
On Mr Okocha’s assertion, probably, borne out of lack of more convincing lies, that nothing is happening in the State with respect to governance, is sure a proof that the man is only acting a bad and an unsellable script to justify the reward of expected gratifying filthy lucre, which is the compelling reason for condescending so low and evilly so. How else is governance measured, if not by executing meaningful and impactful projects, giving hope, inspiring and putting smiles on the faces of the people with joy of fulfilment in their hearts, both civil servants and everyone living and doing business in the State? Is Okocha blind to see and deaf to hear of the good works of the Governor Fubara led Rivers State Government? Civil servants are happy, teachers are highly elated. Several projects are ongoing. Investors are trooping in. The health sector, education, agriculture, sports have been highly boosted under Governor Fubara-led administration. To Okocha, there’s no governance in the State because patronage of free money is not getting to him from the Governor but from other sources that are likely against the Governor.
Let Tony Okocha weep more. Rivers State is breathing fresh air already and is liberated.
Let Tony Okocha tell us how he has, so far, as Rivers State Representative in the Niger Delta Development Commission (NDDC), clearly effected development in the State through the NDDC, and why he lied that there was Cholera outbreak with deaths recorded in Soku in Akuku-Toru Local Government Area with the intent of raking in about ¦ N5billion for non-existent mitigation programmes?
Odike is Special Assistant to Rivers State Governor on Social/New Media .
Bernard C. Idike
-
Business3 days ago
Industry Leaders Defend Local Content, … Rally Behind NCDMB
-

 Niger Delta3 days ago
Niger Delta3 days agoC’River Focused On Youth Empowerment – Commissioner
-
News3 days ago
KENPOLY Appoints Abalubu As Ag. Registrar
-
Rivers3 days ago
NSE Members Tasked On National Dev
-
News3 days ago
UN Warns Floods May Unleash Toxic Chemicals, Pose Risk To Elderly, Ecosystems
-
Business3 days ago
NCDMB Promises Oil Industry Synergy With Safety Boots Firm
-
Politics3 days ago
Your Lies Chasing Investors From Nigeria, Omokri Slams Obi
-
News3 days ago
Police Rescue Kidnapped Victim As Suspects Escape With Gunshots in Rivers

